Dr. Ghohestani’s recommendations on Halloween make-ups for the San Antonio and Boerne Residents!
Halloween is around the corner and if you’re planning to attend a party this year, then chances are you’ll be applying makeup in addition to wearing a costume. Painting your your face for Halloween could be fun, provided your makeup doesn’t harm your skin. According to Dr. Ghohestani, director of Texas Institute of Dermatology, the San Antonio and Boerne clinics, patients with a history of eczema, or asthma are more prone to allergic skin reactions and they have to be very careful about the type of inks used by the artists for facial painting and makeup. Allergic reactions to the cosmetic ingredients in Halloween makeup may initially present with an itchy or a blistery rash. 
Here are our tips for having a wonderful Halloween night without skin rash:
Tip 1. If you’re using a Halloween makeup for the first time, Dr. Ghohestani recommends dabbing a little amount on your forearm first to see if your skin will react. You may repeatedly apply it for few hours then wait for 72 hours. No rash after 72 hours gives you an assurance that the likelihood of reacting to the make-up is very low.
Tip 2. Adding color is a big part of Halloween makeup. But this is your skin not a car or a piece of wood to put the same coloring. Use products designed specifically for the face and avoid using glitter, nail glue or pen markers, as they may damage your skin specially when you try to remove them. Dr. Ghohestani recommends using FDA approved colors. Keep them away from your eyes, if they are not of for that specific purpose. There are two kinds of “glow” effects you might get from Halloween-type makeup: “fluorescent” and “luminescent” (say “loo-min-ESS-ent”) colors, do not use them around the eyes.
Tip 3. Before using any make-up, pay attention if the makeup has a bad smell. In case the make-up smells, avoid using it since it could be contaminated.
Tip 4. Avoid putting too much or a thick layer of makeup. Applying a thick layer may block skin pores and cause acne. Don’t forget to take your oral acne medication(s), the chance that you breakout is relatively high.
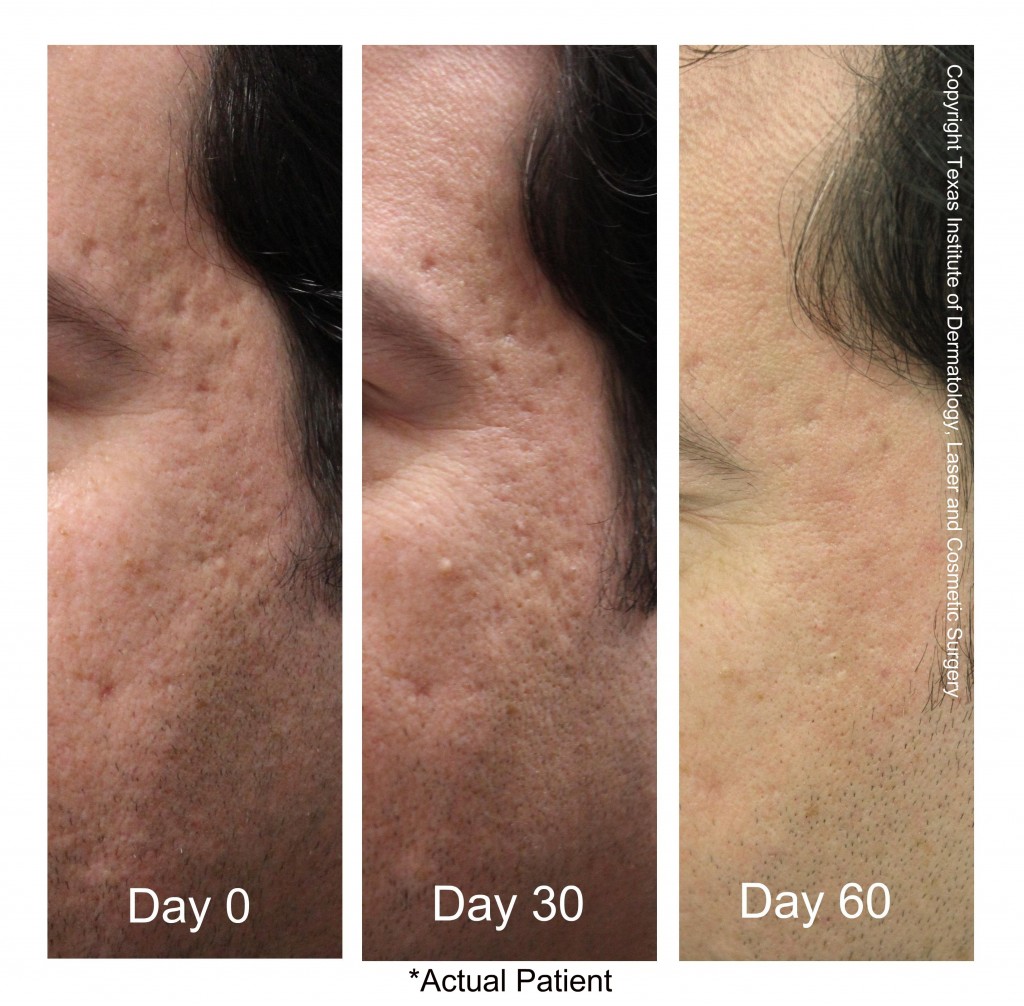
Tip 5. Do not to sleep with your Halloween makeup on, try to wash it off as quickly as you can. Remove it the way the label says. If it says to remove it with cold cream, use cold cream or if it says to remove it with soap and water, then use soap and water. If it says to remove it with eye makeup remover, use eye makeup remover. You get the picture. The same goes for removing glue, like the stuff that holds on fake beards. Importantly, the skin around your eyes is delicate. Remove makeup gently. Moisturize to keep your skin healthy. After washing your face, don’t forget to restore your skin’s hydration by moisturizing. Using a moisturizer to end the night will keep your skin glowing in the morning. Hydroderm, a state-of-the art micro-cleensing system can be used to remove all allergens from the facial pores and the superficial part of the skin. For more information on hydroderm, you may click here.
If you notice itchy, blistery red spots on your skin after removing the make-up call us at 210-698-6777 asap since it could be an allergic reaction.
Halloween Specials!
If you are in San Antonio of Boerne and would like to receive our specials, please email us [email protected]. Contact us by email [email protected] or phone 210-698-6777 to receive our special painless laser hair removal discount, please mention the coupon code: HLWN2014 to receive the limited time offer. ¹ For more information on our state-of the art laser hair removal, please click here.
$199 20 U Botox for one area.
$199 Hdyroderm with a cosmetic consult with M.D. and vitamin C face mask.
$99 Three laser hair removal treatments on one extra-small area. ($600 value). Extra small areas: Ears, Nose, Fingers or Toes.
$199 Two laser hair removal treatments on a small area. ($450 value). Small areas: Chin, Upper lip, Navel, Hands or Feet.
$299 Two laser hair removal treatments on a medium area. ($600 value). Medium Areas: Sideburns, Areolas, Underarms, Front of Neck, Back of the Neck.
$499 Two laser hair removal treatments on a large area. ($900 value). Large Areas: Full face, Forearms, Shoulders, Brazilian, Woman’s Abdomen, woman’s Full Arms or Lower Legs.
$699 Two laser hair removal treatments on an extra-large area. ($1500 value) Upper Legs, Chest, Men’s Abdomen, Lower Back, Upper Back or Men’s Full Arms.
¹ Not valid with any other offer
² Must be active patient or family member of active patient.
3 Must be purchased by Nov 15, 2019













 Do I have to wait for my nail to grow back before I can be treated with the laser for nail fungus? (Manuel – San Antonio)
Do I have to wait for my nail to grow back before I can be treated with the laser for nail fungus? (Manuel – San Antonio)



